World Tuberculosis Day: Solving an Ancient Problem with New Science
UMD’s Volker Briken takes a closer look at the bacteria responsible for causing tuberculosis, one of the world’s deadliest infectious diseases.

Tuberculosis (TB) ravaged civilizations across the globe for thousands of years, with DNA traces of the disease lingering in Neanderthal skeletons dated even as far back as 40,000 B.C.E. Once ominously referred to as “the white death” or “consumption,” the deadly disease was almost invisible because most infections showed no obvious symptoms. Bewildered and afraid, many attributed the disease to anything from atheism to vampirism.
A major breakthrough came on March 24, 1882, when Robert Koch discovered Mycobacterium tuberculosis (Mtb), the bacterial cause of tuberculosis infection in humans. Since then, March 24 has been marked as World Tuberculosis Day and Koch’s work set the stage for several other major milestones in tuberculosis research, including the development of its first vaccine in 1921 and its first antibiotic treatment in 1944.
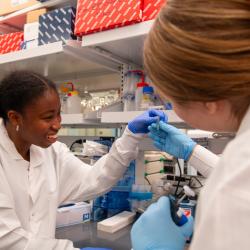
Today, University of Maryland Cell Biology and Molecular Genetics Professor Volker Briken tackles this ancient disease—but with modern scientific approaches.
“We’re interested in finding out how Mtb manipulates our macrophages, a kind of immune cell, for the bacteria to survive in them. It’s a mystery because macrophages usually kill bacteria as soon as they’re detected,” Briken explained. “To do that, we perform genetic screens to discover the importance of Mtb genes for the virulence of the bacteria.”

Briken notes that despite Koch’s groundbreaking discovery over 140 years ago, an effective vaccine to protect adults from tuberculosis still does not exist. In addition, with the rise of antibiotic resistance, traditional treatments are growing more complicated and less effective. As a result, the disease remains a major global threat.
“To the general public, it’s almost unheard of now as an issue in Europe and the U.S. thanks to our infrastructure and surveillance methods, but TB is still a growing problem in many other places in the world. In fact, TB was the deadliest infectious disease globally, only displaced by COVID during the last year or two,” Briken said. “There are more than 10 million people suffering from it right now and 1-2 million people annually dying from it. It’s just mind-boggling numbers for today’s world.”
Laying the foundation for better treatments
Current treatments for tuberculosis are quite limited, according to Briken. Usually, patients are prescribed a cocktail of powerful antibiotics for at least four months. Drug-resistant varieties of tuberculosis lead to more invasive care or higher doses of stronger antibiotics taken over several years, which can sometimes lead to serious side effects like liver failure or even death. The one vaccine that does offer protection against tuberculosis—known as the Bacillus Calmette-Guerin (BCG) vaccine—is targeted toward children and is ineffective for adults.
Briken’s lab is addressing this issue by asking this seemingly simple question: how are Mtb bacteria cells able to survive within macrophages?
“Usually, our macrophages are supposed to kill bacteria, but they’re unable to kill Mtb,” he said. “We’re figuring out what Mtb is doing to those macrophages to survive and how Mtb is manipulating our infected cells on a molecular basis.”
Macrophages are often considered a first line of defense against harmful pathogens because they patrol for foreign bacteria, envelop foreign matter, recognize infections or damaged cells, and then initiate the appropriate immune response. However, Briken and his research team found that Mtb was skillfully exploiting macrophages, hindering crucial components of a healthy immune response.
“One way for a cell to protect itself is to just die—killing itself means taking away the niche, the environment where pathogens can replicate,” he explained. “We found out that Mtb was actually manipulating macrophages to stay alive and identified NuoG, the Mtb gene responsible for inhibiting cell death. If you delete that gene, there would be a lot more cell death and therefore better protection against Mtb.”

Briken’s research on the nuoG gene resulted in special licensing for the improvement of the sole existing tuberculosis vaccine (BCG)and for the potential development of a future vaccine for adults. He’s now researching other genetic elements that could impact natural immune responses against tuberculosis.
Briken and his team identified another Mtb gene (PknF) that inhibits a cell’s ability to induce inflammation as a defense mechanism against infection. Inflammation—like fevers or swelling—is a natural response to harmful pathogens, damaged cells and toxic compounds and begins the healing process.
“If you take a gene away and get a strong phenotype, you can really make a difference,” Briken said. “For example, if we can delete a gene that inhibits a natural immune response from humans, we can potentially improve vaccine capacity.”
Briken is hopeful that his work will pave the way for new protections against the continuing threat of tuberculosis. As he continues his research into Mtb’s evolution and its ability to bypass immune responses, Briken believes that a greater awareness of TB and a collaborative effort to fight it will lead to bigger breakthroughs in other major global health challenges—just as the world came together to overcome past epidemics such as SARS, Ebola and COVID-19.
“The COVID vaccine, especially the speed of its development and implementation, gives me hope that something similar will happen with a vaccine for tuberculosis. It took us about a year to come up with two very effective vaccines and that’s something that’s never happened before in history,” he said. “If we could invest a fraction of the resources mobilized during the COVID-19 pandemic on the tuberculosis problem, we can solve it together.”