Study Reveals How Two Strains of One Bacterium Combine to Cause Flesh-eating Infection
An international team including University of Maryland scientists revealed how genetic variations in a single species of bacteria can amplify infection
In recent years, scientists have found that serious infections that progress rapidly and resist treatment are often caused by multiple microbes interacting with one another. Very little is known about these so-called polymicrobial infections, but traditional diagnostic methods often misidentify them as monomicrobial, or single-microbe, infections.
A new study by a team of scientists that included researchers from the University of Maryland and the University of Texas Medical Branch used genetic analysis to reveal how two different strains of a single species of flesh-eating bacteria worked in concert to become more dangerous than either one strain alone. The study was published in the Proceedings of the National Academy of Sciences on November 11, 2019.
“This research provides clear evidence that a very severe infection considered to be caused by a single species of a naturally occurring bacterium actually had two strains,” said Rita Colwell, a Distinguished University Professor in the University of Maryland Institute for Advanced Computer Studies and a co-author of the study. “One of the strains produces a toxin that breaks down muscle tissue and allows the other strain to migrate into the blood system and infect the organs.”
The original infection—cultured from a patient who developed the severe flesh-eating disease known as necrotizing fasciitis—was diagnosed as a monomicrobial disease. Traditional diagnostics could only determine that the infection was caused by a single species of bacteria called Aeromonas hydrophila. But the disease baffled clinicians when it rapidly turned deadly, requiring a quadruple amputation to save the patient’s life. Through genetic analysis of the culture, Colwell and her team discovered important differences among the individual bacterial cultures that could not be detected through standard diagnostic methods.
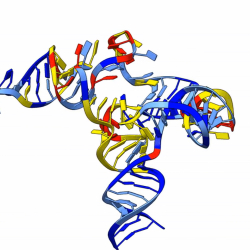
In two previous papers, Colwell and her colleagues isolated and identified two genetically distinct strains of the bacteria that caused the infection. They labeled those strains necrotizing fasciitis 1 (NF1) and necrotizing fasciitis 2 (NF2). In laboratory studies, neither strain produced a deadly infection on its own. But when the strains were combined, the resulting infection became deadly.
In the current study, the researchers manipulated the genetic components of each strain. When they swapped the genetic components that varied between the strains, the team was able to make NF1 behave more like NF2 and visa versa. By testing the mutant strains in mice, the team determined how the genetic variations affected each strain’s ability to cause infection and interact with the other strain.
The three studies combined paint a clear picture of how NF1 and NF2 behave both in separate infections and when combined. In single-strain infections, NF1 remains localized, does not spread to the bloodstream or organs and is cleared by the host immune system. NF2, however, produces a toxin that breaks down muscle tissue and allows it to spread to the bloodstream or organs.
When the strains occur together, the story is reversed. In multi-strain infections, the toxin produced by NF2 breaks down the muscle tissue and enables NF1 to travel to the bloodstream or organs where it becomes deadly. In addition, NF2 remains localized and does not have an opportunity to spread because when it comes in contact with NF1 strains, the NF1 injects a component into NF2 that kills it.
“We’re excited by this very elegant detective work,” Colwell said. “We now have the ability through metagenomics to determine the individual infectious agents involved in polymicrobial infections. With these powerful new methods we can determine how microbes work together, whether they’re bacteria, viruses or parasites.”
The ability to identify the agents involved in polymicrobial infections, whether they are different species or variant strains of a single species, can significantly improve treatment outcomes for infected patients.
“When we treat with a given antibiotic, we’re clearing an organism out of the body,” Colwell said. “But if there’s another organism that’s participating in the infection and that’s also pathogenic, then any antibiotic treatment that doesn’t also target that organism may just be clearing ground for it to grow like crazy.”
Treating only one organism in a polymicrobial infection could be the cause of many secondary infections and chronic infections that resist treatment. According to Colwell, a mixture of antibiotics or therapeutic drugs may be necessary to treat polymicrobial infections. Routinely using the genomic approach that was developed in this study to analyze infections could result in more effectively targeted treatments for diseases caused by polymicrobial infection.
###
Rita Colwell holds a joint appointment as Distinguished University Professor at the Johns Hopkins University Bloomberg School of Public Health and is founder and chair of CosmosID Inc., which performed the metagenomic analysis for this study. In addition to Colwell, Nur A. Hasan, adjunct associate professor in the UMD Institute of Advanced Computer Studies (UMIACS) is a co-author on the paper and the chief science officer for CosmosID, Inc.
The research paper, “T6SS and exoA of flesh-eating Aeromonas hydrophila in peritonitis and necrotizing fasciitis during mono- and polymicrobial infections,” Ana Fernández-Bravo, Paul B. Kilgore, Jourdan A. Andersson, Elizabeth Blears, Maria José Figueras, Nur A. Hasan, Rita R. Colwell, Jian Sha and Ashok K. Chopra was published in Proceedings of the National Academy of Sciences on November 11, 2019.
This research was supported by the National Institutes of Health’s National Institute of Allergy and Infectious Diseases (Award No. AI135453) and the University of Texas John S. Dunn Distinguished Chair in Global Health endowment awarded to Dr. Chopra. The content of this article does not necessarily reflect the views of these organizations.
Writer: Kimbra Cutlip
Media Relations Contact: Abby Robinson, 301-405-5845, abbyr@umd.edu
University of Maryland
College of Computer, Mathematical, and Natural Sciences
2300 Symons Hall
College Park, Md. 20742
www.cmns.umd.edu
@UMDscience
About the College of Computer, Mathematical, and Natural Sciences
The College of Computer, Mathematical, and Natural Sciences at the University of Maryland educates more than 9,000 future scientific leaders in its undergraduate and graduate programs each year. The college's 10 departments and more than a dozen interdisciplinary research centers foster scientific discovery with annual sponsored research funding exceeding $175 million.