Shared Pain, Shared Relief
A new University of Maryland-led study reveals that observing others in pain, even digital avatars, can affect how we feel pain ourselves.
If you sit on a tack, it’s likely to hurt. But pain is more than a physical experience: it’s a phenomenon affected by our emotions, past experiences and the people around us.
Apparently, pain relief is similarly complex.
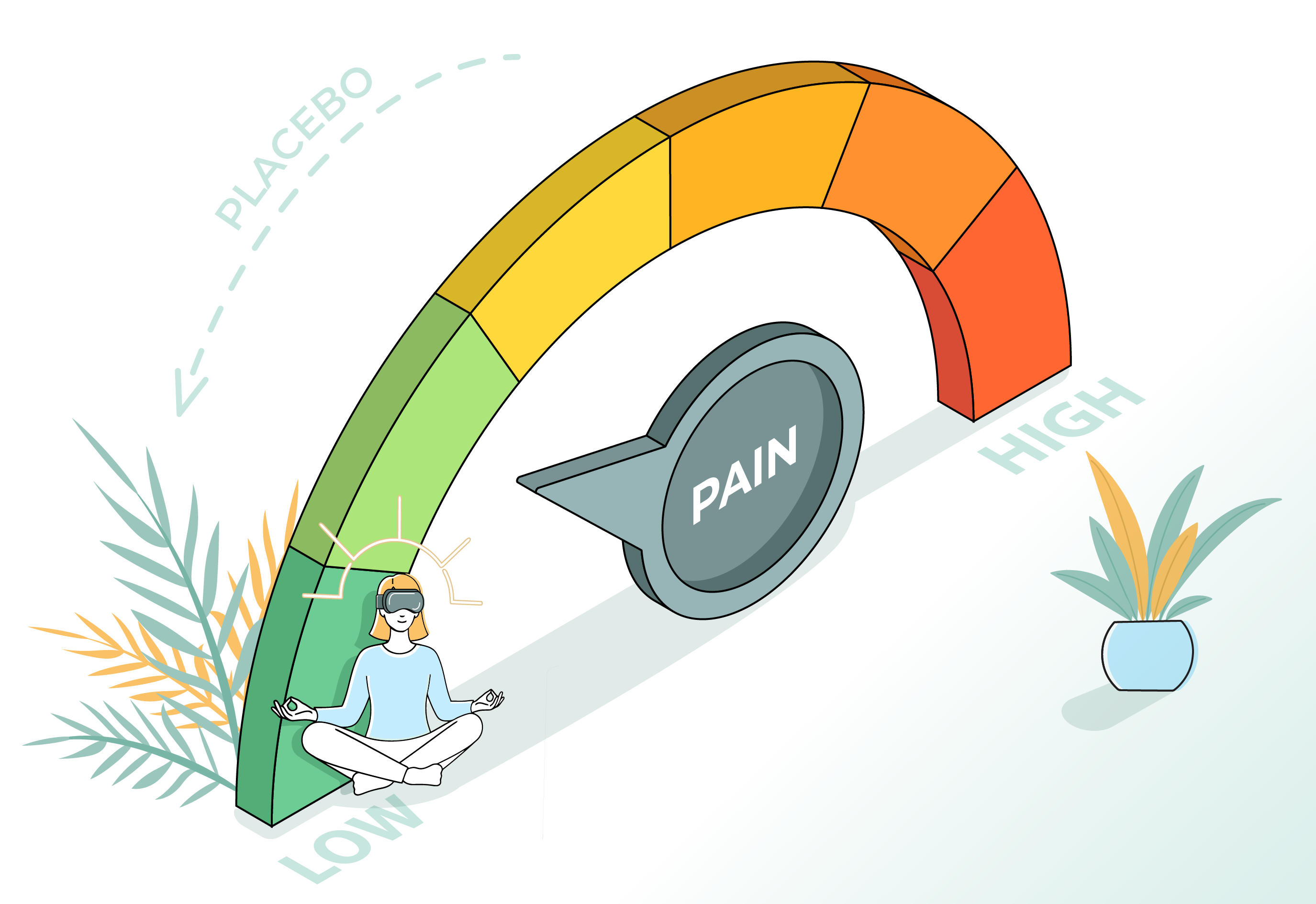
A new study published in Nature’s journal npj Digital Medicine reveals that watching someone else experience pain relief—whether it’s another human or a digital representation of one—can meaningfully reduce the hurt we feel ourselves. But context matters: who we are watching and how they are presented influence the strength of this placebo effect.
For this study, a team led by researchers from the University of Maryland, College Park, and the University of Maryland, Baltimore, investigated how observational vicarious learning—learning by watching others’ therapeutic outcome—can induce first-hand placebo analgesia, a phenomenon in which pain eases without an active treatment.
Participant responses revealed that the placebo effect varied depending on whether the demonstrator receiving control or analgesic cream was a human or an avatar, and whether the individual was presented in immersive virtual reality or standard video. The team’s findings suggest that both avatars and immersive technology can play a role in mediating pain relief through the placebo effect.
“This study provides new insight into how learning from others—across different forms and formats—can shape how we experience pain reduction ourselves,” said Luana Colloca, an MPower Professor of Pain and Translational Symptom Science in UMB’s School of Nursing and director of the Placebo Beyond Opinions Center. “What surprised us most was that immersive virtual environments and even avatars could amplify placebo analgesia. This opens new possibilities for integrating digital tools into pain management strategies.”
Does this hurt? That depends.
In the study, 47 participants watched videos of a human demonstrator receiving painful heat stimulation. Study participants continued to watch as two creams, one blue and one green, were applied to the affected area, and the subject appeared to feel relief from one of them—even though the creams were identical and neither had analgesic properties.
Later, participants received the same heat stimulation and the same two creams. Even without an explicit promise of improvement, participants, using a rating system, reported less pain when using the cream they had seen “work” on the demonstrator, providing evidence that pain relief can be socially learned without overt suggestion.
With the immersive reality expertise of UMCP Computer Science Professor Amitabh Varshney, the researchers also investigated whether study participants’ experiences differed depending on the technology—virtual reality (VR) versus standard 2D video—and whether the demonstrator was an actual human or a digital avatar.
The team found that avatars were significantly more effective at eliciting pain relief in study participants than human actors in immersive VR, whereas human actors produced stronger effects in non-immersive settings. For any clinical application, the work underscores the importance of tailoring digital interventions to the delivery format.
Colloca noted that VR’s ability to “tap into social learning mechanisms” makes it powerful, and that the tool is already being used in clinical settings, from rehab to mental health to medical training. Watching how people engage with virtual systems and understanding the factors that affect their experiences can inform an array of next-generation digital health care tools for pain management and beyond, she said.
Varshney agrees.
“This research shows how VR avatars can inspire empathy and produce powerful placebo effects for pain management in immersive environments. It underscores the vast potential of immersive digital therapeutics to transform health care,” said Varshney, who has a joint appointment in the University of Maryland Institute for Advanced Computer Studies and serves as dean of UMCP’s College of Computer, Mathematical, and Natural Sciences.
###
In addition to Varshney, UMCP authors of the study included Barbara Brawn, Jonathan Heagerty and Sida Li, who also hold appointments in the University of Maryland Institute for Health Computing.
The paper, “Context-dependent placebo hypoalgesia through observational learning: the role of empathy in immersive and non-immersive environments,” by Jewel N. White, Lakota Watson, Yang Wang, Giancarlo Colloca, Jonathan Michael Heagerty, Sida Li, Barbara Brawn, Amitabh Varshney, Roni Shafir, Carmen-Edith Bellei-Rodriguez, and Luana Colloca, was published in npj Digital Medicine on January 27, 2026.
This research was supported by the National Institutes of Health’s National Center for Complementary and Integrative Health (Award No. AT010333). This article does not necessarily reflect the views of this organization.







