Teaming Up to Fight COVID-19
Researchers join forces to develop new drugs for treating coronavirus
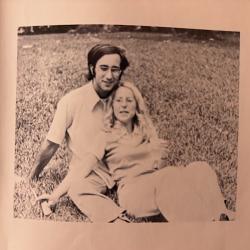
For nearly four years, Assistant Professor Margaret Scull and Professor Jeffrey DeStefano, both from the University of Maryland’s Department of Cell Biology and Molecular Genetics, have worked in close proximity to each other on the third floor of the Bioscience Research Building. And they’re both virologists. But they’ve never collaborated on research—until now.
 Scull studies the human respiratory system and how it defends itself against viral infection. Her lab uses a 3D model of the human airway epithelium to investigate cell activity that can fight viruses. DeStefano works with small molecules called aptamers that bind to structures, such as proteins, to potentially stop infection.
Scull studies the human respiratory system and how it defends itself against viral infection. Her lab uses a 3D model of the human airway epithelium to investigate cell activity that can fight viruses. DeStefano works with small molecules called aptamers that bind to structures, such as proteins, to potentially stop infection.
When the COVID-19 pandemic began, the two started brainstorming how they could combine their efforts to make a difference.
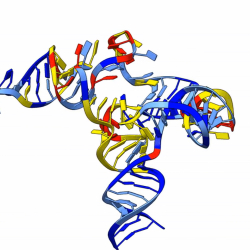
“I had some approaches I thought could be helpful, but I needed other tools to test my lab’s aptamers, which are small pieces of nucleic acid that bind tightly to target proteins,” DeStefano explained. “I wanted to explore the possibility of using some of the things Meg was working on to test my lab’s inhibitors against the coronavirus.”
“I knew Jeff was interested in trying to develop an aptamer to block infection,” Scull said. “It was just a natural step to put two and two together.”
In April 2020, Scull and DeStefano received a $20,000 Coronavirus Research Seed Fund Award from UMD’s Division of Research to do just that. They’ve teamed up in an effort to develop new drugs to treat the novel coronavirus.
 “It will give us enough money to support the personnel that are working on the project as well as establish the platform that we’re planning on using to screen the aptamers that Jeff is developing,” Scull said.
“It will give us enough money to support the personnel that are working on the project as well as establish the platform that we’re planning on using to screen the aptamers that Jeff is developing,” Scull said.
Coronavirus is designated as a biosafety level 3 (BSL3) agent, which means specific protocols must be in place for safety in any lab that works with the virus. Because Scull and DeStefano’s labs do not have the BSL3 infrastructure, their COVID-19 research will take a different approach. They will use pseudoparticles—structures that look like COVID-19, but do not contain the genetic material inside that makes the virus dangerous.
“Basically, from the outside the pseudoparticles look like the regular infectious virus, but on the inside they’re very different,” Scull said. “On the inside of the regular fully infectious virus, you have the viral genome which is required to replicate that virus and make more infectious particles. In the pseudoparticle system, you have genetic information, but instead of encoding coronavirus proteins it encodes what we call a reporter—a protein that’s a particular color or some sort of enzyme that allows us to easily detect when a pseudoparticle gets into a cell. So not only is it a safer tool to use to look at virus entry, but it gives us a really easy readout.”
Scull’s lab is developing a complex cell model of the human airway—a primary target of the coronavirus. The model will be used to screen several different aptamers DeStefano is making to see whether they’re effective in blocking infection in airway epithelial cells.
“I’m trying to make several different aptamers that will essentially be able to bind to the coronavirus surface proteins and perhaps block it from entering the cell,” DeStefano said.
Scull hopes her human airway model can be a game-changer for preliminary drug testing.
“We’re excited to adapt our more physiologically relevant model of the human airway epithelium as a potentially fruitful screening platform for all kinds of inhibitors,” Scull said. “It’s a steppingstone that would give you a better idea of whether your compound was actually going to be efficacious against a virus that targets these cells in your lung.”
If results from this six-month study are encouraging, the first-time collaboration between Scull and DeStefano could lead to further exploration of the potential of aptamers to fight COVID-19 and more.
“There’s only one aptamer that’s been approved for use in humans at this point, so it’s really a burgeoning field,” DeStefano said. “Other people have made these aptamer molecules and have tried to block viruses with them, but I don’t think anyone has been able to bring that completely to fruition as a therapy. I hope that we can contribute to opening up a potentially new direction for treating coronavirus, and perhaps other viruses as well.”